#FreedomFightsFake
This Is Just a Flu
Many Bulgarian public figures have spoken about being sick with COVID-19. Their experience varied — some were seriously ill and even treated in intensive care, though others overcame the disease while experiencing mild or no symptoms. What all of them agree on is that this virus should not be underestimated. In addition, all of them describe the infection as “strange”.
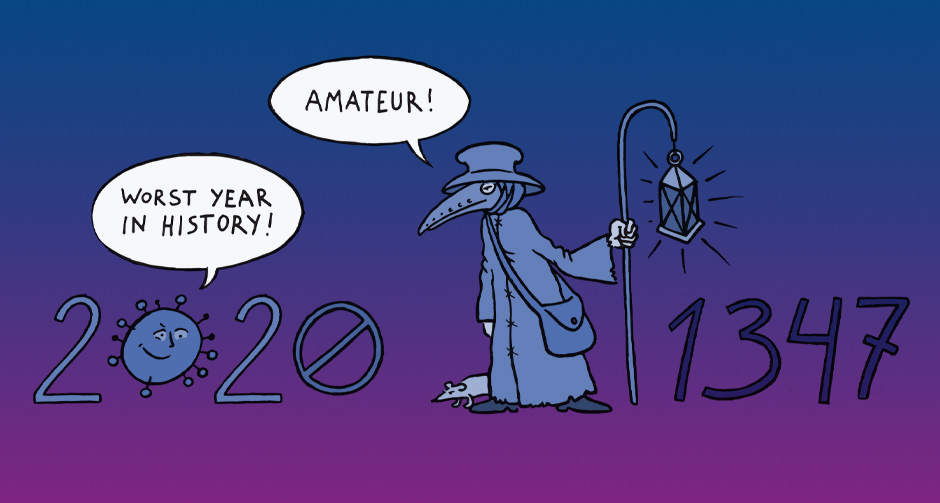
However, in our country and around the world, doubts remain about the seriousness of COVID-19. There are even people who still don’t believe the virus exists.
The new virus is like the seasonal flu — misinformation or optimism
At the beginning of the pandemic, the prevailing view was that the course of COVID-19 would follow that of the seasonal flu. Social networks and forums were saturated with infographics depicting the annual number of deaths from starvation, accidents, cancer, and influenza. The data were used as evidence of how irrelevant the strict restrictions imposed in the fight against the infection were, and as an argument that there was no need to panic. Both around the world and in Bulgaria, high-ranking political leaders and experts supported the notion that SARS-CoV-2 causes the common flu and measures to control it should not be different from those used during seasonal epidemics.
In January, the World Health Organization (WHO) declared the COVID-19 epidemic a public health emergency of international importance. Back then, the disease was ranked as the least dangerous cause of death in a list of nearly 20, which did not even include the most common '"killers" of the world's population: heart disease, stroke, chronic obstructive pulmonary disease, and Alzheimer's. The very real anxiety caused by other well-known, widespread infections compared to the lack of an imminent sense of threat from COVID-19 made the new infection seem ordinary to many people. Not for long.
Is COVID-19 a respiratory disease?
Despite initial hypotheses that SARS-CoV-2 was just another coronavirus that causes seasonal respiratory disease, significant challenges treating the seriously ill prompted scientists to start searching for answers in other directions. A series of studies have found that the virus can actually affect any organ, including the circulatory system. The theory that COVID-19 is an inflammation of the vascular system (vasculitis), rather than a respiratory disease, was popularized in Bulgaria mostly by a pulmonologist, Dr Alexander Simidchiev, whose media appearances received wide attention. Dr Simidchiev and other medical experts have made attempts to dispel the notion of the disease as "mild", "respiratory", and "seasonal."
However, despite all the research evidence, the analogy with seasonal respiratory diseases continues to circulate as a legitimate point of view, even in scientific debate on the subject. Among the major arguments put forward by its proponents is that the data gathered so far on the spread and mortality of this disease are more similar to those of influenza than to severe infections such as rubella and measles. One of the supporters of this idea in Bulgaria is the chairman of the Center for the Protection of Healthcare Rights, Dr Stoycho Katsarov. From the very beginning of the pandemic, Dr Katsarov has focused on the actions in response to the infection, which according to him, pose greater risks than the disease itself.
Since this opinion is based on some actual facts, it calls to account the actions of official authorities not only in our country, but all over the world. It sounds like a reasonable and logical viewpoint. This theory, however, fails to acknowledge a key detail — at the core of the aggressive measures against the spread of SARS-CoV-2 is not what science knows about the virus, but what it doesn’t.
“Lethality” and “Severity of the disease”
How many of those infected with the new coronavirus become seriously ill? And how many die?
The values of these two measures is an indication of the severity of a disease. The Ebola virus, for example, is extremely alarming because this year's epidemic killed about half of those affected, and mortality over the years has varied between 25 and 90 percent.
It’s still difficult to accurately calculate the prevalence, severity, and mortality of COVID-19 since the disease is new. In early August, WHO published a scientific letter explaining in detail the principle for determining the mortality of this disease. Researchers explained that two different measures were observed: the IFR (infection fatality ratio), which is the ratio of the number of deaths to the total number of infected people, and the CFR (case fatality ratio), or lethality, which is the number of deaths to the number of confirmed cases. Due to the differences in the calculation of the two indicators, the estimated "mortality" varies from 0.1percent to more than 25percent.
On the other hand, the very calculation of the possible number of patients is based on assumptions. To illustrate this problem, Our World in Data published a chart including data from the United States on confirmed cases of coronavirus and an estimate of the true number of patients according to four of the most widely used mathematical models. All four models show that the number of those infected probably exceeds the number of confirmed cases. However, when it comes to the exact number of infections and the way the disease develops over time, the models offer completely different results.
In many academic papers, scientists note that significant age differences must be considered, which means that simply averaging lethality across data sets would lead to incorrect conclusions.
One can define a case of COVID-19 as “severe” if it fits certain medical criteria outlined by international professional organizations. Among the most clearly recognized symptoms by non-specialists is respiratory failure. There is still no clear scientific consensus on how likely it is for a coronavirus patient to fall severely ill. The reason is that in addition to age groups, other factors have been determined as producing differences, such as pre-existing conditions and even by country.
A medical journal, the Lancet, in a recent publication predicts that about 4 percent of the world's population is at risk of developing severe COVID-19. The risk for men (6 percent) is two times bigger than that for women (3 percent). The share for vulnerable groups is highest in countries with aging populations, African countries with a high prevalence of HIV/AIDS, and small island states with a high prevalence of diabetes. A key factor in risk assessment is the presence of diabetes and chronic kidney, cardiovascular, and respiratory diseases.
At this stage of the pandemic, mathematical models cannot offer accurate answers. But the nine months since the corona crisis began has been enough to show that this new disease can cause long-term problems.
Evidence of this illness lasting 10,12, or even more than 15 weeks has appeared in different parts of the world. Such cases have also been documented by the news media and described on social networks. Science has confirmed some of COVID-19’s long-term complications and ruled out others. Although we have already learned a great deal about the virus, many of the questions concerning the course of the disease remain unanswered.
Thus, currently available information on the proportion of deaths and survivors of severe cases may not be sufficient for a comprehensive assessment of the seriousness of the disease. However, one thing is for sure — it’s becoming increasingly difficult to categorize COVID-19 as a “mild cold”.
The long-term effects of COVID-19 and why they are important
One of the most prestigious hospitals in the US, the Mayo Clinic, recently published an article explaining the most serious long-term confirmed complications of COVID-19 discovered so far. The article highlights that most of the patients fully recover within a few weeks. But in other cases, even those of patients with mild COVID-19, the symptoms don’t disappear, even after an initial recovery. Most often, patients continue to suffer from fatigue, cough, shortness of breath, headaches, and joint pain. The Mayo Clinic team also lists the vulnerable organs and systems: the heart, lungs, brain, and circulatory system.
The initial belief that the disease doesn’t pose much risk to young, healthy people is also refuted. The Clinic’s examination of mild cases is particularly challenging for physicians, since many patients report some symptoms long after their official recovery.
However, insufficient, and in some places, missing diagnostics hinder the study of subsequent complications. For example, a survey conducted in the Netherlands revealed that almost three months after their first symptoms appeared, 9 out of 10 people reported having problems performing normal daily activities. Of the survey’s participants, 1,622 people suspected of having coronavirus, 91 percent were not hospitalized and 43 percent were not diagnosed by a doctor at all.
A study by King's College London estimated that only 52 percent of COVID-19 patients in the UK recovered in less than 13 days. The study included both severe cases treated in intensive care units and people with mild symptoms who tackled the disease at home. Another study in the UK, published in Brain, a specialized neurology journal, reported damage to the nervous system caused by COVID-19. The study also showed that there was no correlation between the severity of the illness and some of its later complications.
The authors examined patients without any respiratory symptoms and found that neurological disorders were their first and only symptom of COVID-19. They documented cases of 43 people between the ages of 16 and 85 with various forms of brain damage due to the infection.
Last summer, the British channel Sky News reported on a hospital in the Italian city of Bergamo, one of the most affected areas in the world at that time. Local doctors were monitoring the condition of people treated for COVID-19 during the worst weeks of the epidemic in March and April. Italian doctors told the channel that psychosis, insomnia, kidney disease, spinal infections, strokes, chronic fatigue, and motor problems were among the most serious complications, and evident even after the patients had been cured. They believe that COVID-19 is a systemic infection that affects all organs in the body, not a mere respiratory disease, as was thought at the beginning of the pandemic. The proactive search for positive cases of coronavirus was provoked by a previous small study, which showed that over 87 percent of patients continue to suffer from at least one COVID-19 symptom even after they are considered cured.
Like any other new phenomenon, this disease gives rise to its own vocabulary. The cases described above receive the common name “long COVID”. This concept arose spontaneously after countries with widespread prevalence, such as the United Kingdom and the US, saw many cases of patients reporting long-term malaise well after their treatment had ended.
The concept has also been adopted by the medical community. In early September, the prestigious British Medical Journal even organized a webinar for specialists advising them on how to diagnose and treat patients with “long COVID”.
Seriously, but not hopelessly
The absence of specialized treatment for the many patients with long-term symptoms has prompted specialists to seek alternative solutions for them. A CNN report from the European Respiratory Society International Congress highlighted a study that gives hope for faster recovery through targeted motor and respiratory rehabilitation. One curious detail is that rehabilitation has a positive impact even on psycho-neurological symptoms such as depression and anxiety.
We must not forget, however, that not all questions about COVID-19 have been answered. Also, it’s possible that new research on the subject will once again change the understanding of physicians about the nature of the disease, its course, and its treatment.
About the author: Nadezhda Tsekulova is a freelance journalist and a communication expert, based in Sofia Bulgaria.
This article is part of the Infodemics’ Chronicle from Bulgaria, which is under the umbrella of the global #FreedomFightsFake campaign of FNF. The campaign is in cooperation with the Association of European Journalists in Bulgaria. Find the article in the original in Bulgarian here: